The
sodden grass quickly soaked through the denim fabric of my shoes. No umbrella could save my feet in this
rain. Good thing this cemetery isn’t too
big, I thought. This is sort of like
looking for a needle in a haystack, but the graves have to be here,
somewhere. I looked at my shoes and my
soaking feet. No way were they going to
dry on the hour and a half drive I had to make to get home. What was I doing here in a cemetery in Hyde
Park, Utah (nearly 100 miles from home) on a rainy Saturday afternoon,
anyway?
For as
long as I can remember, my family has gathered and gone to visit cemeteries,
usually in conjunction with Memorial Day weekend. The Murray City Cemetery was a favorite when
I was young, as monuments stretched over my head. I was fascinated by these tall tributes to a
life lived and lost. We ran freely among
the headstones, but my father taught us not to climb on the inviting grave
markers.
Memorial
Estates became a mainstay in my family after the death of my brother in
1976. For a time, we visited the
cemetery weekly, on Sundays. Week after
week we arrived at the cemetery to find a flower on my brother’s grave. We never knew who placed it there. But every week we knew that someone
remembered him, and it was a great gift of comfort to us.
The
list of graves to visit at Memorial Estates grew to include four former
classmates (two died in the 5th grade, one passed away in high school,
and another died at the age of 22, shortly after her marriage). Family also began filling the plots near my
brother’s resting place: my
grandparents, my aunt, my infant cousin.
The South Jordan Cemetery became a regular on the visit list as well. There we decorated graves for my father-in-law, his mother,
and other relatives, I began wandering this cemetery looking for my husband’s
ancestors who had settled this place and raised their families before ending up here, beneath the lawn. My children and I meandered through the headstones, reading names, looking for ones familiar from genealogy
charts and family stories. "If it is a Holt, Beckstead, or Newbold," I told my
kids, "they are related to you!"
I began
visiting graves on vacations and other trips:
the Tomb of the Unknown Soldier in Washington, D.C.; the Old Pioneer
Burial Ground in Nauvoo, Ill.; JFK’s grave in Arlington National Cemetery; Charles Lindbergh's grave on Maui; Sacagawea on the Wind River Reservation in Wyoming (ok, so many historians
believe this is not really Sacagawea's burial place, but it is still a beautiful
cemetery); and the grave of Georges Seurat and other famous people in Pere
LaChaise in Paris, France. I have walked
through small cemeteries off the side of the road, or in small towns. I have read inscriptions and epitaphs. I love cemeteries. They are beautiful and
peaceful, and it is fascinating to me how we choose to honor our dead.
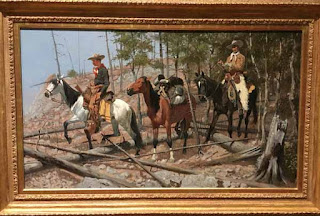
Seurat Family Tomb in Paris
Once I
stood, plat number and map in hand, and tried to find an ancestor in the
Salt Lake City Cemetery, but William Lewis escaped me. No matter how hard I looked, I could not find
his grave. The day was long, and we were
all getting tired, so we left. Fast
forward a couple of years, and I was back looking for William Lewis. And there was a tall monument to him, and
other family members. Pretty hard to
miss! I have no idea why I couldn’t find
it the first time, but I was happy to see it.
It felt like quite a victory to finally locate his grave.
I love
the chase. I love finding the marker,
the place where my family member lies in repose. I love putting together pieces of
information. I soak in the sorrow and
solemnity when an infant lies alone in a plot, no family nearby, or when a
family has lost child after child to early death. Cemeteries are a wealth of information. They
are also an art exhibit, filled with poems and prose, sculpture and carvings.
I had
to go to Logan to visit the Utah State University campus that Saturday. Prior to my visit, I remembered my mom telling me about
relatives buried in the Logan area. A
quick search of the Findagrave website (a blessing to family history
researchers everywhere!), informed me that Luther C. Burnham was buried in
Hyde Park. It wasn't far from the USU campus and there might be time to visit once I was through in Logan....
So
maybe now you can understand how I ended up in Hyde Park with soaking shoes in
the rain. I held the umbrella and the
camera and looked at one marker, and then the next. Not this one. Not that one. I kept looking. “Here it is!
He’s here!” I exclaimed. My great-great grandfather. I snapped a few pictures, looked at this
beautiful place, and took a moment in the rain before returning to the car to
shed my wet shoes and dry my feet.
Luther C. Burnham headstone
It is
more than the love of the chase that made me drive from Logan to Hyde Park in
the rain that day before returning home to Salt Lake. It is the love of family. It is the connectedness I feel extending
through generations, linking my ancestors and my children. In cemeteries, I see not only monuments to
individuals, but stories of family. And
finding my great-great grandfather's headstone in Hyde Park was worth the soaking wet shoes.